Abstract
Background:Hepatitis-associated aplastic anemia (HAAA) is known as a rare variant of acquired aplastic anemia, characterized by a syndrome of bone marrow failure following the development of hepatitis. Immunosuppressive therapy (IST) or hematopoietic stem cell transplantation (HSCT) could provide lifesaving opportunities for severe HAAA patients. However, to date, no cohort has characterized treatment outcome and long-term survival between those patients receiving IST and HSCT. In this study, we aim to retrospectively evaluate the outcome of these two therapies for severe HAAA in China.
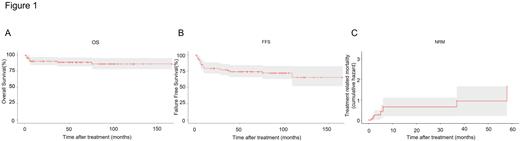
Methods: Patients consecutively diagnosed as severe HAAA between August 2008 and Jan 2021 were enrolled in this study. The definition of severe HAAA is that severe aplastic anemia developed within three months after documented hepatitis. The enrollments were patients who received HSCT or IST as a first-line treatment. Patients with HSCT were conditioned as described previously with cyclophosphamide (Cy, 120-150 mg/kg, divided doses on days -6 to -2), and rabbit ATG (Thymoglobulin®, Genzyme, Cambridge, MA) (2.5mg/kg once i.v. daily on days -6 to -2) or p-ALG (Anti-lymphocyte Immunoglobulin®, Wuhan Institute of Biological Products Co., Ltd., China) (20mg/kg once i.v. daily on days -6 to -2), Fludarabine 150 mg/m2 i.v.in divided doses on days -6 to -2, with or without Busulfan (Bu, 0.8 mg/kg four times i.v. daily on days -7 and -6). IST consisted of both rabbit ATG (rATG) (3~3.75mg/kg once i.v. daily on 5 days), porcine antilymphocyte globulin (pALG)(20mg/kg once i.v. daily on 5 days), combined with a six-month course of cyclosporine (3mg per kilogram per day orally, with adjustment of the dose to maintain a blood level between 200 and 400 ng per milliliter). Probabilities of overall survival (OS), failure-free survival (FFS), and treatment-related-mortality (TRM) were calculated by Kaplan-Meier method.
Results and Discussion: This study retrospectively included 94 consecutive HAAA patients, including 68 patients underwent HSCT and 26 patients receiving IST. The IST and HSCT groups were similar with respect to age and gender ratio. The median follow up were 1752 (±153.62, 95%CI 1450.90~2053.10) days, and 2648 (±321.41, 95%CI 2018.05-3277.96) days among alive patients in the IST and HSCT group, respectively. In HSCT group, all patients achieved neutrophil engraftment. No primary or secondary graft failures (GF) was documented. Compared with patients receiving alternative donor HSCT (n=11), patients in matched sibling donor HSCT (MSD-HSCT) group (n=15) had a significant lower cumulative incidence of acute graft versus host disease (aGVHD) (20±10.33% vs 56.4±15.47%, p=0.048), and lower incidence of cytomegalovirus (CMV) reactivation group (72.73% vs 13.33%, p=0.004). No clinical significance of chronic graft versus host disease (cGVHD) incidence group (43.4±18.85% vs 50±35.4%, p=0.78) and bacterial/fungus infection (26.67% vs 36.36%, p=0.683) was found between MSD-HSCT group and alternative donor-HSCT. Attributable causes of death were pneumonias and severe infection in patients receiving HSCT. In IST group, the hematology response rate to treatment evaluated at 3m, 6m and 12m was 27.68%, 52.94%, and 60.23%, respectively. There were thirteen patients were non-evaluable, including six patients transferred to perform HSCT, two patients were diagnosed MDS/AML transformation and one patient relapsed. The 5-year overall survival (OS) and failure-free survival (FFS) rate was 85.5±4.44% (95% CI, 0.772, 0.946) and 69.6± 5.35% (95% CI, 0.599,0.809) of all enrolled HAAA patients, respectively (Figure 1). For patients receiving different therapy, the 5-year OS rates were 92.86 ± 6.88% in MSD-HSCT group, 72.7± 13.43% in alternative donor-HSCT, and 84.1 ± 7.28% in the IST group (P = 0.56). Otherwise, the 5-year estimated FFS rate was 56.0± 11.51% in the IST group, compared with 92.86 ± 6.88% in the MSD-HSCT group and 72.7± 13.43% in alternative donor-HSCT group (P = 0.10). The cumulative incidence of treatment-related-mortality (TRM) of MSD-HSCT, alternative-HSCT and IST was 7.1±6.9% (95% CI, 80.30-100), 27.3±13.4% (95% CI, 50.60-100), 14±5.54% % (95% CI, 7.58-97.6) (p=0.22), respectively. Even there was no difference between the HSCT and IST groups in OS, MSD-HSCT group still showed superior FFS. Patients receiving alternative donor HSCT, and IST showed comparable OS and FFS.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal